“Why Am I in Pain? And What Can I (and You) Do About It?”
This question is one that I think the profession of physical therapy is uniquely positioned to help people understand! For individuals with musculoskeletal, nerve injury, or pain related to hypersensitivity of the nervous system, physical therapy may be one of the best choices to treat their pain and restore them to a better level of movement health and functional mobility.
In Part 1 of this series (Part 1: How to Talk to Patients in Pain), I introduced some of the fundamental concepts of pain neuroscience education, the use of language, and some basic definitions and functions of pain. In Part 2 of this series, I want to dig in to trying to answer the questions above. The question, “Why Am I in Pain?” gets at the idea that we want to try to identify a root cause of pain, or mechanism. The second question prompts us to think about matching treatments to that proposed cause for best chances at resolution. To guide our thinking in these areas, I will present an introduction to a “Mechanisms-Based Approach,” to evaluating potential causes or drivers of an individual’s pain and provide a preview for Part 3: Treating Complex Pain Presentations in Physical Therapy.
You won’t want to miss Part 3, which will be a discussion of some tips and approaches to addressing long-lasting, persistent/chronic, or recalcitrant pain.
What Are Pain Mechanisms?
The idea of pain mechanisms refers to the idea that the etiology of pain can be diverse and complex. Ideally, we want to find a root cause of pain instead of just identifying and treating pain as a symptom. As discussed in Part 1 of this series, pain is a perception (i.e., different than a sensation) and can have multiple contributors to why we experience it including tissue damage (or not), emotions, memories, environment, nerve sensitivity, perceived danger/threat from our nervous system and many others. We have a better chance of treating pain effectively in physical therapy (and all medical pursuits) if we better understand the dominant causes or mechanisms behind a person’s pain experience.
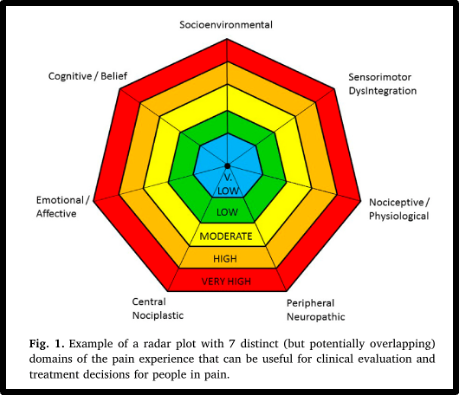
One of the most widely accepted descriptions of pain mechanisms comes from physical therapist and researcher, Dr. Kathleen Sluka, PT, PhD and her research collaborators. Dr. Sluka has a vast amount of experience and research in the field of pain mechanisms, and literally “wrote the book” on the topic: Mechanisms and Management of Pain for The Physical Therapist. Within this approach, three dominant pain mechanisms are described with two background factors of a person’s motor system and psychosocial factors (see diagram below from Chimenti, 2018 article).

The three dominant pain mechanisms and brief descriptions of each are these:
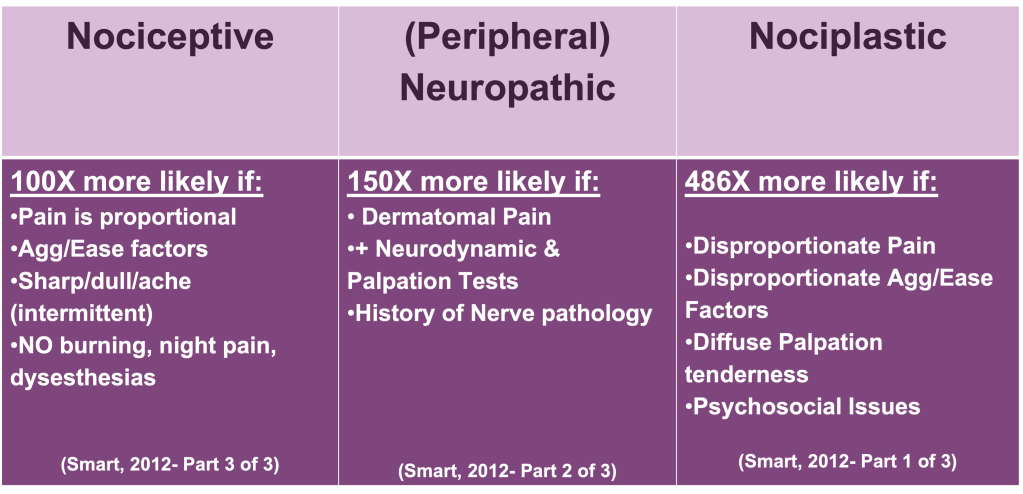
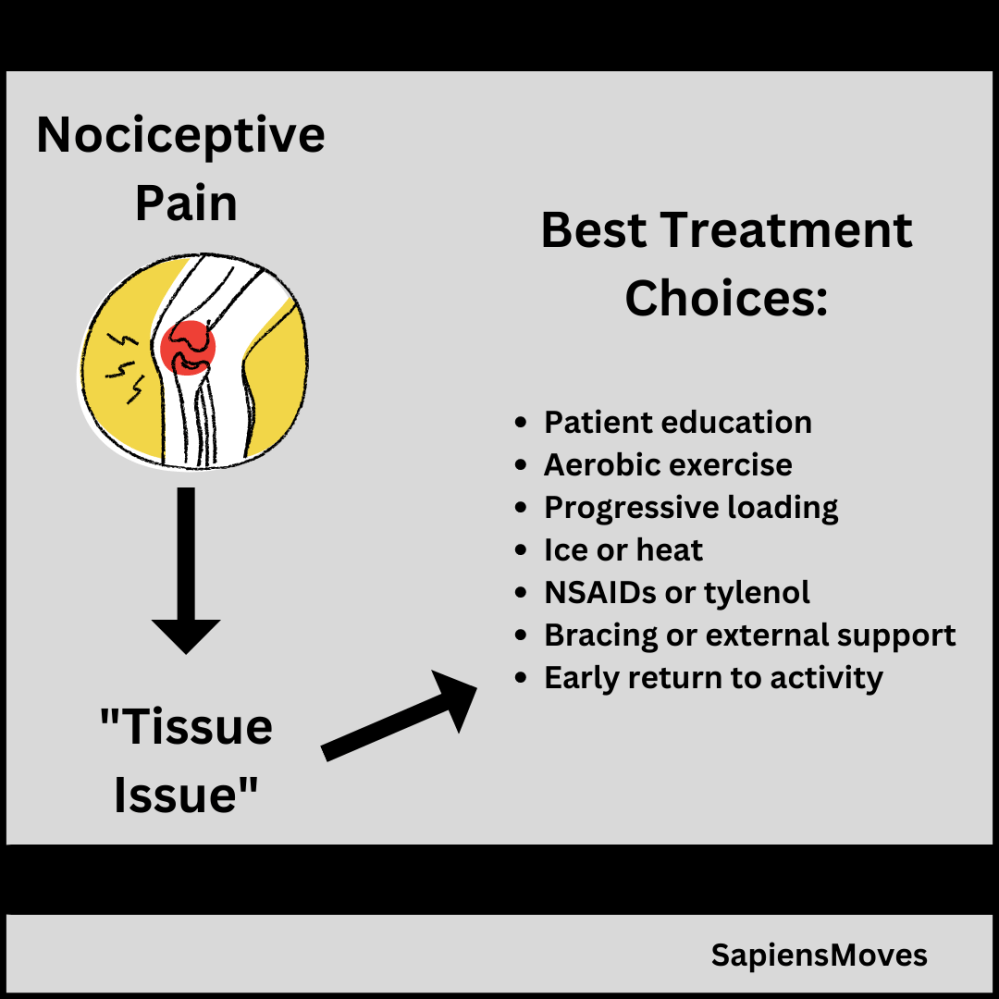
- 1. Nociceptive Pain: “The most common human experience of pain” (Kosek, 2016), Nociceptive pain refers to pain due to activation of nociceptors and is often linked to local tissue damage or perceived tissue damage. It tends to behave how we would expect pain to behave: it comes and goes, is proportional to tissue loading, has predictable factors that make it better and make it worse, and tends to be sharp or dull but not burning or marked by severe dysesthesias (Chimenti, 2016; Kosek, 2016; Smart, 2012).
- 2. Neuropathic (Peripheral) Pain: This type of painis what you might think of as “nerve pain,” and is usually related to an injury to a nerve or group of nerves. It feels like burning or could manifest as numbness, tingling, or reduced sensation in an area. Common findings with this type of pain are history of nerve injury and positive neurodynamic or palpation tests (i.e., pulling or pushing on the nerve provokes symptoms).
- 3. Nociplastic Pain: This type of pain is the hardest to describe and it is thought to be due to changes in the nervous system that increase sensitivity and/or affect how inputs to the nervous system are processed and produce pain as an output. This type of pain is harder to describe and can be more diffuse, have less predictable factors that may make it better or worse, and is often not proportional to the amount of tissue loading. There could also be a strong prevalence of psychosocial contributors and often this is the pain that persists and causes significant distress to an individual.
An extreme simplification (but perhaps quick way to remember) these different types of pain is this:
Nociceptive = Tissue Injury
Neuropathic = Nerve Injury
Nociplastic = Processing Dysfunction
See the chart below that I adapted from the work of Keith Smart and colleagues who performed elegant factor analyses to identify common findings from each of these three categories of dominant pain mechanisms (Smart, 2012):
As we seek to evaluate and treat pain within a biopsychosocial approach the “background factors” may become more or less prominent contributors to a person’s pain experience. Research supports that health, illness, and YES- Pain! to be impacted by a complex interplay of genetics/epigenetics, biology, psychology, and social factors (Zimney, 2023).
Another representation of pain mechanisms further “maps” some of these factors in what has been described as a seven factors, radar plot diagram (Walton et al., 2018). As you can see below in this diagram of pain mechanisms, there is a delineation of some of the psychosocial and environmental contributors as Emotional/Affective, Cognitive/Belief, Socio/Environmental, and includes the factor of Sensorimotor disintegration to acknowledge the impact of dysfunction in sensory and/or motor systems that is likely with pain. See below for the diagram of this radar plot (from Walton et al., 2018):
Matching Treatments to Pain Mechanisms
As you can see, representing an individual’s pain presentation or pain experience with these breakdowns of likely contributions can help us better understand the potential cause(s) of their pain and also have a better chance at successfully treating it; both with physical therapy treatments and with other medical treatments. This way, patients and medical providers can better answer the questions that patents often have of:
“What Can I (and You) Do About It (my pain)?”
In physical therapy, common treatments for pain could include exercise, manual therapy, and modalities like heat, ice, electrical stimulation, or dry needling. Certain types of treatments may be better suited for different types of pain and the table and infographic below are some ideas and treatment considerations that I use to guide my treatments based on what I think my patient’s dominant pain mechanism may be.
Treatment Choices Based on Dominant Pain Mechanism:
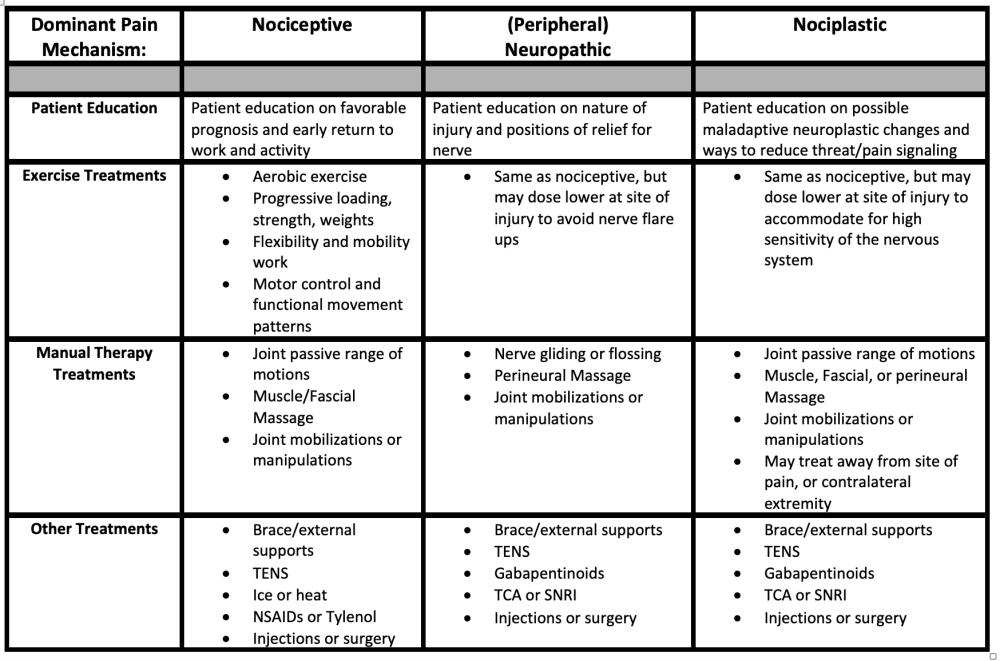
When selecting the types of manual therapy to use in a physical therapy setting for these different pain mechanisms, it may also be useful to have a better understanding of the proposed mechanism of effect from the manual therapy treatment technique! Furthermore, selecting the appropriate level of force or intensity and duration of application cannot be understated. A fantastic resource to learn more about this type of treatment selection and understanding comes from Physical therapist, researcher, and fellow of the American Academy of Orthopedic PT, Dr. Carol Courtney, PT, PhD, ATC, FAAOMPT who has co-authored a course of study and clinical practice guideline discussing some of the evidence behind different mechanisms of manual therapy. (Courtney, 2021).
I hope that this post has been informative and interesting to better help you understand how pain works and how we can better treat pain. For a more in depth discussion of the treatment techniques that I mentioned above for treating more “tricky” types of pain such as neuropathic and nociplastic… Stay tuned for Part 3 of this series, where I will discuss the topic of “Treating Complex Pain Presentations in Physical Therapy”
References:
- Chimenti RL, Frey-Law LA, Sluka KA. A Mechanism-Based Approach to Physical Therapist Management of Pain. Physical therapy. 2018;98(5):302–314.
- Courtney CA, Fernández-de-las-Peñas C. Manual Therapy for Chronic Conditions: A Mechanistic Approach to Modern Manual Therapy. Published online 2021. Academy of Orthopedic Physical Therapy.
- Kosek E, Cohen M, Baron R, et al. Do we need a third mechanistic descriptor for chronic pain states? Pain. 2016;157(7):1382-1386. doi:10.1097/j.pain.0000000000000507
- Sluka, KA. Mechanisms and Management of Pain for the Physical Therapist. Philadelphia; Wolters Kluwer Health; 2nd edition; 2016.
- Smart KM, Blake C, Staines A, Thacker M, Doody C. Mechanisms-based classifications of musculoskeletal pain: Part 1 of 3: Symptoms and signs of central sensitisation in patients with low back (±leg) pain. Manual Therapy. 2012;17(4):336-344.
- Smart KM, Blake C, Staines A, Thacker M, Doody C. Mechanisms-based classifications of musculoskeletal pain: Part 2 of 3: Symptoms and signs of peripheral neuropathic pain in patients with low back (±leg) pain. Manual Therapy. 2012;17(4):345-351.
- Smart KM, Blake C, Staines A, Thacker M, Doody C. Mechanisms-based classifications of musculoskeletal pain: Part 3 of 3: Symptoms and signs of nociceptive pain in patients with low back (±leg) pain. Manual Therapy. 2012;17(4):352-357.
- Walton DM, Elliott JM. A new clinical model for facilitating the development of pattern recognition skills in clinical pain assessment. Musculoskeletal Science and Practice. 2018;36:17-24.
- Zimney K, Van Bogaert W, Louw A. The Biology of Chronic Pain and Its Implications for Pain Neuroscience Education: State of the Art. JCM. 2023;12(13):4199. doi:10.3390/jcm12134199
2 Comments Add yours