Within any group of runners–long distance runners, track runners, recreational or competitive runners—some of the most commonly reported injuries are “shin splints” and stress fractures in the leg or foot (Nattiv, 2012). As you may expect, the majority of stress fractures, estimates 80% or greater occur in the lower body (Kahanov, 2015; Matcuk, 2016). So, what exactly are the causes of these injuries? Are they dangerous? And what is the difference between a stress fracture and “shin splints”?
Part 1: Classifying “Bone Stress Injuries” and Tips for Prevention
In this post, I’d like to explore these ideas and also talk about ways to reduce the risk for these injuries. In Part 2 of this series, I will discuss treatment progressions and factors guiding safe timelines for return to running.
Classifying “Bone Stress Injuries”:
Stress fractures and “shin splints” fall into a broader category of what has been termed “Bone Stress Injuries”.
Bone Stress Injuries can be classified based on (Warden, 2014):
- Clinical findings (signs and symptoms)
- Location (“High-Risk” vs. “Low-Risk” site)
- “Grade” of injury based on MRI findings
It has been proposed that these injuries occur along a continuum of severity. See Figure Below:

Stress Reactions:
This is the least severe category of “Bone Stress Injury” (BSI) and when located at the shin or tibia is often termed “shin splints” or “Medial Tibial Stress Syndrome” (MTSS). Stress reactions affect the bone at the point where muscles attach to it (i.e., periosteum) and often show up on MRI as mild periosteal edema (Warden, 2014).
“Shin splints”, though a broad diagnostic term that is sometimes inconsistently used, usually refers to an overuse injury or irritation of the periosteum where muscles attach to the tibia. This is commonly observed with the muscles at the posteromedial tibia: the tibialis posterior, flexor digitorum, and soleus and so is also called “Medial Tibial Stress Syndrome” (MTSS). Some findings that you would NOT suspect to see in this condition are anterior tibial (front of shin) pain–focal tenderness at the anterior tibia may be more indicative of a stress fracture; and neurovascular complaints (i.e., numbness, tingling, or color changes), which may be more indicative of lower leg compartment syndrome (Galbraith, 2009).
Stress Fractures:
A stress fracture refers to a small crack or cracks in a bone that occur due to small micro trauma or repetitive loading over time. They often will not go completely through the bone and are usually too small to show up on an X-Ray (though evidence of stress fracture healing—a bone callus, could show up on an X-Ray). To differentiate a stress reaction from a stress fracture, clinical severity is evaluated (i.e., severity of pain, loading tolerance, etc.), and an MRI may be performed. In a stress fracture, you will be more likely to see a fracture line on MRI.
Complete Fractures:
A complete fracture refers to a crack in bone that passes all the way through the bone and is often visible on X-Ray (and MRI). This type of BSI is the most severe category and will take the longest to heal. Clinically, a runner with a complete fracture will have more localized and severe pain and have much less load tolerance (e.g., probably is unable to run and even walking could hurt!).
The most common site for stress fractures in runners is in the tibia (about 25% of all stress fractures, Kahanov, 2015). Let’s take a look at injury severity along the continuum by comparing findings from a person with “shin splints” (Tibial Stress Reaction) versus a Tibial Stress Fracture. In both of these types of BSI, you may expect to see a history of repetitive “overuse” or “overload” and often a change in running frequency, intensity, or environmental factors such as training surfaces or footwear. Individuals will often report pain with impact loading (painful running, duh!), which is why they are probably seeking out physical therapy care in the first place!
Check out the table below for key clinical findings that my help to differentiate between these two types of BSI:
| “Shin Splints”
(aka “Medial Tibial Stress Syndrome”) |
Tibial Stress Fracture
|
| Pain RESOLVES after stopping activity (usually)
|
Pain LINGERS after stopping activity |
| Pain = Mild, DIFFUSE ache | Pain = Moderate to Severe , sharp, LOCALIZED
|
| Pain with palpation at POSTEROMEDIAL Tibia | Pain with palpation at ANTERIOR Tibia OR POSTEROMEDIAL Tibia
|
| Palpation tenderness at MUSCLE, edge of bone
|
Palpation tenderness at BONE |
| No pain with unloading the limb | Pain with “unloading” the limb
(Shifting weight OFF of that limb) |
| Swelling is unlikely
|
Swelling could be present |
| Findings based on: Patel, 2011; Reinking, 2017; Tenforde, 2016, Warden, 2014 and author’s clinical experience | |
For a great discussion of tips for evaluating an athlete with “shin splints”, check out this podcast with: Dr. Zach Long, PT, DPT: (PT on ICE Daily Show Podcast #749: Assessment of Athletes with ‘Shin Splints’).
The location of a BSI can help to guide management and prognosis. A BSI classified as “Low-Risk” is located on the compression side of the bone’s bending axis and generally has a good natural course of healing with few complications. While a “High-Risk” BSI is on the tensile side of bending axis and could be at risk for non-union or progression to full fracture (Warden, 2014). This will be discussed more in Part 2 because it will guide treatment progression (Spoiler Alert: “Low-Risk” BSIs can be progressed more quickly to return to sport/running vs. “High-Risk”).
See table below for “Low-Risk” vs. “High-Risk” sites for BSI:
|
Low and High-Risk Bone Stress Injuries in Runners (Adapted from Warden, 2014) |
|
|
“Low-Risk” Sites |
“High-Risk” Sites |
|
Posteromedial Tibia |
Anterior Cortex of the Tibia |
|
Fibula/Lateral malleolus |
Medial Malleolus (Tibia) |
|
Femoral Shaft, Pelvis |
Femoral Neck |
| Calcaneus |
Talus, Navicular |
| 2nd to 4th Metatarsals
(diaphysis) |
5th Metatarsal (Proximal diaphysis) 2nd Metatarsal (Base) Sesamoid bones of great toe |
Finally, BSIs can be classified or “Graded” based on the severity of imaging findings. As mentioned above, the imaging modality of choice to evaluate bone stress injuries is MRI because of its high sensitivity (ability to rule out other conditions) and specificity (ability to rule in fracture) as well as the fact that it does not confer radiation exposure risks like X-Rays and bone scans (Fredericson, 1995; Galbraith, 2009; Kahanov, 2015). X-Rays usually cannot detect signs of acute stress fractures such as bone cortex changes or bone marrow edema if taken within 2-3 weeks and so may have limited utility in management decisions.
See figure below for Pros and Cons of different imaging techniques (Kahanov, 2015):
Classification of BSIs based on MRI findings follows a “Grading” system based on severity: from least severe, a “Grade 1” to Most severe, a “Grade 4b”; and is based on presence or absence of edema at the periosteum and bone marrow. Also note that 4a and 4b are distinguished by the presence or absence of a fracture line.
See table below for this MRI grading system (originally reported for Tibial BSIs). (From Matcuk, 2016):
Tips for Preventing Bone Stress Injuries
Our first goal in treating bone stress injuries, should be PREVENTION! At the very least, once we suspect this type of injury in a runner, being proactive in managing load and training variables can reduce the risk of progression to a more serious injury (remember the continuum above?!) Understanding the etiology (cause) of bone stress injuries and risk factors for these injuries can help to improve our success in preventing these injuries.
“Our first goal in treating bone stress injuries should be prevention”
-Leda McDaniel, PT, DPT
The main proposed cause of BSIs is an “overload” at the bone and surrounding tissues that happens because of repetitive microtrauma. The load felt at these tissues is dependent on loading “cycles” and rate. Translated to running, this means how frequently and how far does the individual run (days per week and mileage) and how fast. If we can understand that each of these variables can contribute to the “stress” (force) and “strain” (deformation) that the bone feels–then it naturally follows that manipulating these variables can help in our prevention efforts!
Bone “stress” (i.e., force), “strain” (i.e., deformation or change in length), AND “damage” is actually a positive thing in measured doses because each of these things stimulate positive remodeling and strengthening of bone. For example, targeted remodeling of bone at an area of microdamage can lead to reduced bone strain (deformation) from the same load (“stress”) (Warden, 2014). That means that the bone becomes more resilient! Pretty cool, huh?!
But, just like with other training paradigms and injury prevention, we want to optimize dose to allow for positive adaptations and recovery (see figure below):

In normal bone, the remodeling triggered by loading keeps pace (like that runner pun?), with the damage occurring from loading and the system self regulates to equilibrium. However, if loading exceeds the threshold for remodeling, then this cycle may be thrown out of balance and perpetuate bone injury.
One interesting finding that to me hammers home this link between loading and bone response is this: Due to differences in foot strike patterns in distance runners (tend toward rearfoot or “heel strike”) versus sprinters (tend towards forefoot strike) and the force felt on the foot and leg: distance runners are at greater risk for long bone stress fractures at the leg (i.e., tibia, fibula, femur), while sprinters are more at risk for foot stress fractures (i.e., tarsals, metatarsals, etc.) (Bennel, 1998).
Factors that have shown to increase risk for BSIs include:
- High training volume: Running > 25 miles per week for recreational runners* (Patel, 2011)
- Faulty biomechanics: (runners with BSI had greater vertical GRF loading rate and peak acceleration, Warden, 2014). Increased pronation and reduced flexibility of calf muscles (gastrocnemius, soleus) have also been seen more often in those with MTSS (Galbraith, 2009). Higher navicular drop (Reinking, 2017)
- Increased rearfoot eversion with walking (Kinoshita, 2019)
*Not ALL studies show this as increasing risk! One study showed weekly mileage for runners was NOT linked with increased risk for BSI (Reinking, 2017)
Some Factors that Increase Risk may be “Non-Modifiable”, these include:
- Female sex (Reinking, 2017)
- Hormonal state* (Warden, 2014)
- Medication use (Warden, 2014)
*Note: With all bone injuries (especially stress fractures) it would be wise to screen for “RED-S” (Relative Energy Deficiency Syndrome, formerly referred to as “The Female Athlete Triad”), asking questions about history of stress fractures, nutrition and eating habits and potentially referral to nutritionist or psychologist as needed. In this syndrome, poor nutrition can lead to reduced energy availability <> hormonal changes <> bone mineral density changes.
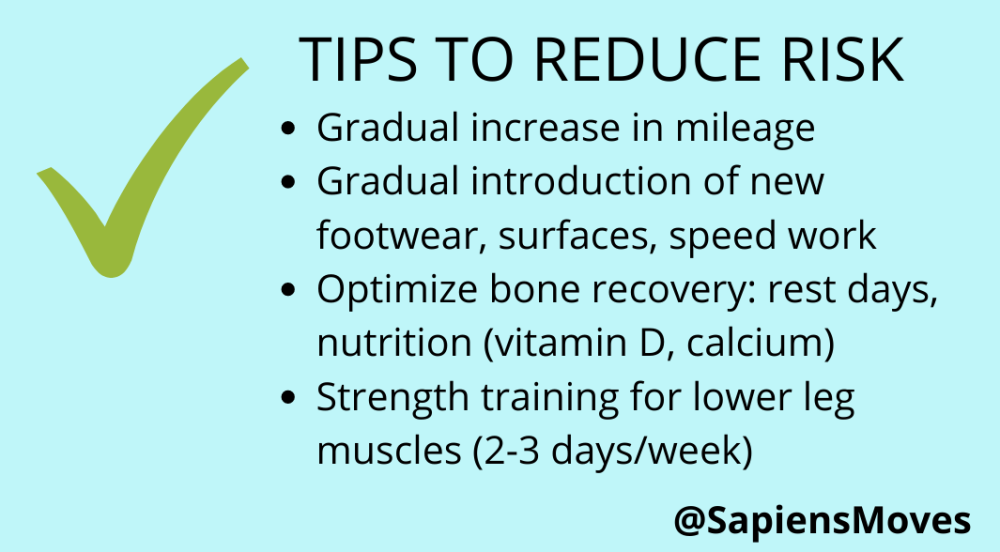
Thus, in order to reduce risk of BSI, recommendations may include modifying the risk factors that we have control over: gradually introducing changes to training volume and environment, optimizing bone recovery, and creating strength in the muscles of the legs that may reduce “overload” at the bones susceptible to these injuries.
There is some evidence to suggest (in military personnel) that “shock-absorbing” insoles may reduce the risk for bone stress injuries (Patel, 2011; Shaffer, 2006), though it is unclear whether this is true for other populations of runners and active individuals.
FREE INFOGRAPHIC DOWNLOAD: PREVENTING BONE STRESS INJURIES IN RUNNERS

Check out Part 2: Treating Bone Stress Injuries where I discuss recovery timelines and treatment strategies for bone stress injuries in runners.
References:
- Bennell, KL, Malcolm, SA, Thomas, SA, Wark, JD, & Brukner, PD. The Incidence and Distribution of Stress Fractures in Competitive Track and Field Athletes: A Twelve-Month Prospective Study. The American Journal of Sports Medicine. 1996; 24(2), 211–217.
- Dobrindt O, Hoffmeyer B, Ruf J, et al. Estimation of return-to-sports-time for athletes with stress fracture – an approach combining risk level of fracture site with severity based on imaging. BMC Musculoskelet Disord. 2012;13(1):139.
- Fredericson M, Bergman AG, Hoffman KL, Dillingham MS. Tibial Stress Reaction in Runners: Correlation of Clinical Symptoms and Scintigraphy with a New Magnetic Resonance Imaging Grading System. Am J Sports Med. 1995;23(4):472-481.
- Galbraith RM, Lavallee ME. Medial tibial stress syndrome: conservative treatment options. Curr Rev Musculoskelet Med. 2009;2(3):127-133.
- Kahanov L, Eberman L, Games K, Wasik M. Diagnosis, treatment, and rehabilitation of stress fractures in the lower extremity in runners. Open Access J Sports Med. 2015; 6:87-95.
- Kijowski R, Choi J, Shinki K, Del Rio AM, De Smet A/ Validation of MRI classification system for tibial stress injuries. AJR Am J Roentgenol. 2012; 198(4):878–884.
- Kinoshita K, Okada K, Saito I, et al. Alignment of the rearfoot and foot pressure patterns of individuals with medial tibial stress syndrome: A cross-sectional study. Physical Therapy in Sport. 2019;38:132-138.
- Liem BC, Truswell HJ, Harrast MA. Rehabilitation and Return to Running After Lower Limb Stress Fractures: Current Sports Medicine Reports. 2013;12(3):200-207.
- Matcuk GR, Mahanty SR, Skalski MR, Patel DB, White EA, Gottsegen CJ. Stress fractures: pathophysiology, clinical presentation, imaging features, and treatment options. Emerg Radiol. 2016;23(4):365-375.
- Nattiv A, Kennedy G, Barrack MT, et al. Correlation of MRI Grading of Bone Stress Injuries With Clinical Risk Factors and Return to Play: A 5-Year Prospective Study in Collegiate Track and Field Athletes. Am J Sports Med. 2013;41(8):1930-1941.
- Patel DS. Stress Fractures: Diagnosis, Treatment, and Prevention. 2011;83(1):8.
- Reinking MF, Austin TM, Richter RR, Krieger MM. Medial Tibial Stress Syndrome in Active Individuals: A Systematic Review and Meta-analysis of Risk Factors. Sports Health. 2017;9(3):252-261.
- Shaffer SW, Uhl TL. Preventing and treating lower extremity stress reactions and fractures in adults. J Athl Train. 2006;41(4):466-469.
- Tenforde AS, Kraus E, Fredericson M. Bone Stress Injuries in Runners. Physical Medicine and Rehabilitation Clinics of North America. 2016;27(1):139-149.
- Warden SJ, Davis IS, Fredericson M. Management and Prevention of Bone Stress Injuries in Long-Distance Runners. J Orthop Sports Phys Ther. 2014;44(10):749-765.


Hi Leda-
Just wanted to encourage you that you’re doing great work with this kind of content! I have a runner who I am wanting to screen for/ manage who is on the BSI spectrum, and this is a very concise and helpful post! Keep them coming!
LikeLike